As How to Understand the Connection Between Hormones and Sleep takes center stage, this opening passage beckons readers into a world where the intricate dance between our body’s chemical messengers and our nightly rest is illuminated. We will explore the profound ways in which hormones orchestrate our sleep-wake cycles, influencing everything from when we feel tired to the quality of our slumber.
This exploration delves into the primary hormonal players, including melatonin, cortisol, sex hormones, thyroid hormones, and growth hormone, detailing their specific roles and how their delicate balance or imbalance can significantly impact our sleep patterns. Understanding these connections is the first step toward achieving more restful and rejuvenating nights.
Introduction to Hormones and Sleep Regulation
Hormones act as the body’s master chemical messengers, orchestrating a vast array of physiological processes. Among their most critical functions is the regulation of our natural sleep-wake cycle, a complex biological rhythm that dictates when we feel alert and when we feel drowsy. This intricate interplay between hormones and sleep is fundamental to maintaining overall health and well-being.The precise timing and release of hormones are largely governed by our internal biological clock, known as the circadian rhythm.
This approximately 24-hour cycle influences numerous bodily functions, including hormone secretion, body temperature, and metabolism. Disruptions to this rhythm, whether from shift work, travel, or lifestyle choices, can significantly impact hormone balance and, consequently, sleep patterns.Several key hormones play a direct and substantial role in influencing the quality and duration of our sleep. Understanding their functions and how they interact is crucial for appreciating the intricate biological mechanisms that underpin restful sleep.
The Circadian Rhythm and Hormone Release
The circadian rhythm is a powerful internal timekeeper that synchronizes our body’s functions with the external environment, primarily the light-dark cycle. Specialized cells in the brain’s hypothalamus, known as the suprachiasmatic nucleus (SCN), receive light signals from the eyes and relay this information to other parts of the brain and body, thereby dictating the timing of various physiological events, including hormone release.This rhythm dictates the pulsatile release of many hormones throughout a 24-hour period.
For instance, hormones that promote wakefulness tend to be released during daylight hours, while those that facilitate sleep and rest are secreted as darkness falls. This synchronized release ensures that our bodies are prepared for the demands of wakefulness and the restorative processes of sleep.
The suprachiasmatic nucleus (SCN) acts as the master circadian pacemaker, receiving photic input and orchestrating a cascade of hormonal signals that govern sleep-wake cycles.
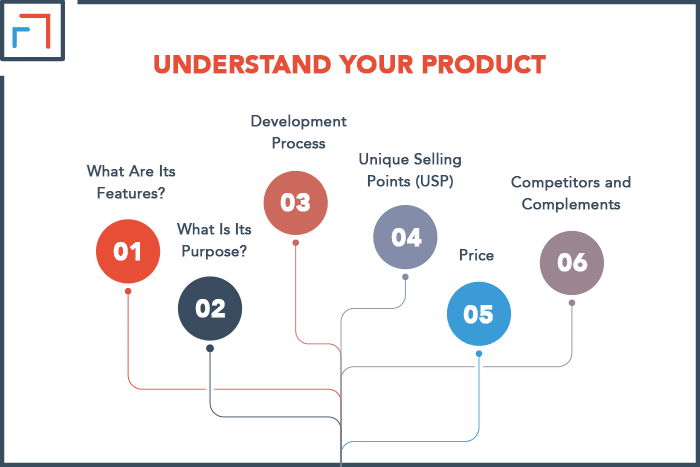
Primary Hormones Impacting Sleep
A variety of hormones directly influence our ability to fall asleep, stay asleep, and experience restorative sleep. These hormones work in concert to create the optimal internal environment for sleep.The following hormones are particularly influential in sleep regulation:
- Melatonin: Often referred to as the “sleep hormone,” melatonin is produced by the pineal gland. Its production is suppressed by light and stimulated by darkness, signaling to the body that it is time to sleep. Melatonin levels typically begin to rise in the evening, peak in the middle of the night, and decline towards morning.
- Cortisol: This stress hormone plays a vital role in the body’s stress response and energy regulation. Cortisol levels naturally follow a circadian pattern, being highest in the morning upon waking and gradually decreasing throughout the day, reaching their lowest point around midnight. A healthy cortisol rhythm is essential for initiating sleep.
- Growth Hormone (GH): Released primarily during deep sleep stages, growth hormone is crucial for cell repair, muscle growth, and bone development. Its release is strongly linked to the restorative phases of sleep, highlighting the importance of sufficient and quality sleep for physical recovery.
- Ghrelin and Leptin: These hormones regulate appetite and satiety. Ghrelin, the “hunger hormone,” tends to increase when sleep-deprived, while leptin, the “satiety hormone,” may decrease. This hormonal imbalance can lead to increased cravings and altered eating patterns, which can indirectly affect sleep.
Key Hormones Influencing Sleep
Understanding the intricate dance of hormones within our bodies is fundamental to grasping how we fall asleep, stay asleep, and wake up feeling refreshed. While many hormones play a role, one stands out as the primary conductor of our sleep-wake cycle. This section delves into the pivotal hormone responsible for signaling to our bodies that it’s time to rest.The regulation of our circadian rhythm, the internal biological clock that dictates sleep and wakefulness over a 24-hour period, is a complex interplay of various physiological signals.
Among these, hormonal messengers are paramount, with one specific hormone acting as the principal architect of sleep initiation.
Melatonin: The Sleep Hormone
Melatonin is a hormone produced by the pineal gland, a small endocrine gland located deep in the brain. It is often referred to as the “sleep hormone” because its primary function is to regulate the body’s circadian rhythms, specifically signaling the onset of darkness and promoting sleep. Melatonin doesn’t force sleep, but rather creates the optimal physiological conditions for it by influencing our internal clock.
Physiological Triggers for Melatonin Production and Release
The production and release of melatonin are primarily driven by the absence of light. As daylight fades, specialized photoreceptor cells in the retina detect the decrease in ambient light. These cells send signals to the suprachiasmatic nucleus (SCN) in the hypothalamus, which is the body’s master clock. The SCN then communicates with the pineal gland, stimulating it to begin synthesizing and secreting melatonin.
Conversely, when light is detected, the SCN signals the pineal gland to suppress melatonin production.
Typical Daily Fluctuation of Melatonin Levels and Sleepiness
Melatonin levels naturally follow a predictable daily pattern, directly influencing our perception of sleepiness. Throughout the day, melatonin levels are typically very low. As evening approaches and light diminishes, melatonin production begins to rise, gradually increasing throughout the night. This rise in melatonin is what signals to the body that it is time to wind down and prepare for sleep.
Peak melatonin levels usually occur in the middle of the night, coinciding with the deepest stages of sleep. As morning approaches and light returns, melatonin levels begin to fall, contributing to the feeling of wakefulness. This ebb and flow of melatonin is crucial for maintaining a healthy sleep-wake cycle.
Impact of Light Exposure on Melatonin Secretion
Light, particularly blue light emitted from electronic devices like smartphones, tablets, and computers, has a significant impact on melatonin secretion. Exposure to bright light, especially in the hours leading up to bedtime, can suppress melatonin production and delay its release. This suppression can make it harder to fall asleep and can disrupt the natural rhythm of the circadian clock. Even dim light can have an effect, though less pronounced than bright light.
Therefore, minimizing light exposure in the evening, and creating a dark sleep environment, is essential for optimal melatonin function and good sleep hygiene.
Key Hormones Influencing Sleep: Cortisol
Cortisol, often referred to as the “stress hormone,” plays a crucial role in regulating our body’s natural sleep-wake cycle, also known as the circadian rhythm. While essential for alertness and energy, its intricate relationship with sleep can become disruptive if not properly managed. Understanding cortisol’s diurnal pattern and its impact on sleep quality is key to achieving restful nights.Cortisol is produced by the adrenal glands and its release is primarily controlled by the hypothalamus and pituitary gland in the brain.
This hormone is vital for numerous bodily functions, including metabolism, immune response, and helping the body cope with stress. Its influence on sleep is directly tied to its cyclical release throughout the day.
Cortisol’s Diurnal Pattern
Cortisol levels follow a predictable daily rhythm, peaking in the morning and gradually declining throughout the day to their lowest point in the evening. This pattern is a fundamental aspect of our internal biological clock.The typical diurnal pattern of cortisol levels is as follows:
- Morning Peak: Cortisol levels begin to rise in the early morning hours, even before waking, reaching their highest point shortly after waking up. This surge is responsible for helping us feel alert and ready to start the day. This is often referred to as the cortisol awakening response (CAR).
- Gradual Decline: After the morning peak, cortisol levels steadily decrease throughout the day. This gradual decline signals to the body that it is time to wind down and prepare for sleep.
- Evening Trough: By late evening and throughout the night, cortisol levels are at their lowest, which is conducive to falling asleep and staying asleep.
Disruption of Sleep by Elevated Cortisol
When cortisol levels remain elevated, particularly in the evening or at night, it can significantly interfere with the ability to fall asleep and maintain sleep. This disruption is due to cortisol’s alerting and energizing effects, which are counterproductive to the relaxation needed for sleep.Factors that can lead to elevated cortisol at night include:
- Chronic Stress: Persistent psychological or physical stress triggers a sustained release of cortisol, overriding the natural evening decline. This can lead to a state of hyperarousal, making it difficult to relax and fall asleep.
- Irregular Sleep Schedules: Shift work, jet lag, or inconsistent bedtime routines can desynchronize the body’s natural cortisol rhythm, leading to elevated levels when sleep is desired.
- Certain Medical Conditions: Conditions like Cushing’s syndrome or chronic pain can also contribute to persistently high cortisol levels.
- Stimulant Intake: Consuming caffeine or engaging in intense exercise close to bedtime can also increase cortisol levels and disrupt sleep.
The consequence of elevated nighttime cortisol is often characterized by difficulty initiating sleep (sleep onset insomnia), frequent awakenings during the night, and a feeling of not being well-rested upon waking.
Managing Cortisol Levels for Better Sleep
Fortunately, several lifestyle strategies can help manage cortisol levels and promote better sleep. The goal is to support the natural diurnal rhythm of cortisol, ensuring it is high in the morning and low at night.Effective methods for managing cortisol include:
- Stress Reduction Techniques: Incorporating mindfulness, meditation, deep breathing exercises, or yoga into your daily routine can significantly lower stress and, consequently, cortisol levels. Even short periods of these practices can be beneficial.
- Consistent Sleep Schedule: Maintaining a regular sleep-wake cycle, even on weekends, helps to regulate the body’s internal clock and cortisol rhythm. Aim to go to bed and wake up around the same time each day.
- Regular Physical Activity: While intense exercise close to bedtime can elevate cortisol, moderate and regular physical activity during the day can help reduce overall stress and improve sleep quality.
- Healthy Diet: Consuming a balanced diet rich in fruits, vegetables, and whole grains, while limiting processed foods, sugar, and excessive caffeine, supports overall hormonal balance.
- Exposure to Natural Light: Getting adequate exposure to natural sunlight, especially in the morning, helps to reinforce the circadian rhythm and can aid in regulating cortisol production.
- Relaxing Bedtime Routine: Establishing a calming pre-sleep routine, such as taking a warm bath, reading a book, or listening to soothing music, signals to your body that it’s time to wind down, helping to lower cortisol levels before bed.
By actively managing these factors, individuals can help their bodies adhere to the natural cortisol rhythm, thereby fostering an environment conducive to restorative sleep.
Key Hormones Influencing Sleep: Sex Hormones (Estrogen and Progesterone)

While cortisol plays a significant role in wakefulness, the intricate dance of sex hormones, particularly estrogen and progesterone, profoundly impacts sleep architecture and quality in women. These hormones exhibit cyclical fluctuations throughout the menstrual cycle, and their shifts during specific life stages like pregnancy and menopause can lead to noticeable changes in sleep patterns. Understanding these hormonal influences is crucial for appreciating the unique sleep experiences of women.The interplay between estrogen and progesterone is central to regulating various bodily functions, including sleep.
Their levels rise and fall predictably, influencing neurotransmitter activity in the brain, such as serotonin and GABA, which are vital for sleep initiation and maintenance. These hormonal shifts can alter the duration of sleep stages, the frequency of awakenings, and overall subjective sleep quality.
Estrogen’s Influence on Sleep Architecture and the Menstrual Cycle
Estrogen, primarily produced by the ovaries, has a complex and often biphasic effect on sleep. Its influence varies depending on its concentration and the phase of the menstrual cycle. Generally, higher estrogen levels are associated with improved sleep quality, including increased slow-wave sleep (deep sleep) and reduced awakenings. Conversely, lower estrogen levels can lead to disrupted sleep.Throughout the menstrual cycle, estrogen levels rise during the follicular phase, peaking just before ovulation.
This period is often associated with more consolidated and restorative sleep. Following ovulation, during the luteal phase, estrogen levels remain relatively high before declining sharply if fertilization does not occur, leading to menstruation. This premenstrual decline in estrogen, alongside rising progesterone, can contribute to premenstrual sleep disturbances.
Progesterone’s Impact on Sleep During Pregnancy and Menopause
Progesterone, also produced by the ovaries, is often described as having a sedative effect, promoting sleepiness. Its levels increase significantly after ovulation and remain high during pregnancy, which can contribute to increased daytime sleepiness and changes in sleep patterns. During pregnancy, women often experience more frequent awakenings, particularly in the later trimesters, due to physical discomfort, hormonal changes, and increased urination.Menopause marks a significant decline in both estrogen and progesterone.
The drop in progesterone, in particular, is strongly linked to sleep disturbances experienced by many women during this transition. Reduced progesterone can lead to a decrease in slow-wave sleep and an increase in wakefulness, contributing to insomnia and fragmented sleep. Hot flashes, another common menopausal symptom, can also severely disrupt sleep.
Typical Sleep Patterns During Different Hormonal Phases in Women
The typical sleep patterns experienced by women can vary significantly across different hormonal phases:
- Menstruation: During menstruation, both estrogen and progesterone levels are low. This can sometimes be associated with more fragmented sleep and a subjective feeling of poorer sleep quality, though this can vary greatly among individuals.
- Follicular Phase (pre-ovulation): As estrogen levels rise, sleep quality generally improves. Women may experience more consolidated sleep and feel more rested.
- Ovulation: Estrogen peaks around ovulation, and sleep is typically at its best during this phase.
- Luteal Phase (post-ovulation): Progesterone levels rise, and while this can initially promote sleepiness, the subsequent decline in both estrogen and progesterone towards the end of the luteal phase (premenstrual period) can lead to increased sleep disturbances, including difficulty falling asleep and staying asleep.
- Pregnancy: Early pregnancy may see increased sleepiness due to high progesterone. Later pregnancy often involves fragmented sleep due to physical discomfort, hormonal shifts, and increased need to urinate.
- Menopause: The significant decline in sex hormones, especially progesterone, is a major contributor to sleep disturbances, including insomnia, frequent awakenings, and worsened sleep quality.
Potential Sleep Disturbances Associated with Hormonal Shifts in Women
Hormonal shifts in women can manifest in various sleep disturbances:
- Insomnia: Difficulty falling asleep or staying asleep is a common complaint, particularly during the premenstrual phase, pregnancy, and menopause.
- Fragmented Sleep: Frequent awakenings throughout the night, leading to a feeling of unrefreshing sleep. This is often seen in later pregnancy and during menopause.
- Excessive Daytime Sleepiness: While sometimes associated with increased progesterone in early pregnancy, it can also be a consequence of poor nighttime sleep quality.
- Sleep Apnea: Hormonal changes, particularly the decline in progesterone during menopause, may increase the risk or severity of obstructive sleep apnea in women.
- Restless Legs Syndrome (RLS): While not solely hormonal, RLS symptoms can be exacerbated by hormonal fluctuations, especially during pregnancy.
Key Hormones Influencing Sleep: Thyroid Hormones
The thyroid gland, a small butterfly-shaped organ located at the base of your neck, plays a crucial role in regulating your body’s metabolism. This metabolic control is intricately linked to sleep regulation, meaning imbalances in thyroid hormones can significantly disrupt sleep patterns. Understanding this connection is vital for achieving restorative sleep.Thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3), influence virtually every cell in the body.
They affect heart rate, body temperature, and energy expenditure, all of which are fundamental to the sleep-wake cycle. When these hormones are not produced in the correct amounts, the body’s internal clock and sleep architecture can be profoundly affected.
Thyroid Hormone Levels and Sleep Regulation
The thyroid gland’s output of hormones influences the central nervous system’s ability to initiate and maintain sleep. Thyroid hormones are thought to interact with neurotransmitter systems involved in sleep, such as serotonin and norepinephrine, and to modulate the body’s response to circadian rhythm cues. Disruptions in these delicate balances can lead to a range of sleep disturbances.
Hypothyroidism and Sleep Disturbances
Hypothyroidism, a condition where the thyroid gland does not produce enough thyroid hormones, is often associated with increased sleepiness and fatigue. While it might seem counterintuitive, this excess sleepiness doesn’t necessarily translate to restful sleep. Individuals with hypothyroidism may experience longer sleep durations but report feeling unrefreshed upon waking. This is because the overall metabolic slowdown can impair the quality of sleep, leading to less time spent in deeper, restorative sleep stages.Common sleep symptoms associated with hypothyroidism include:
- Excessive daytime sleepiness
- Difficulty waking up
- Feeling groggy and unrefreshed after a full night’s sleep
- Increased need for sleep
- Sleep apnea, particularly obstructive sleep apnea, can be more prevalent due to reduced muscle tone in the airway
Hyperthyroidism and Sleep Disturbances
Conversely, hyperthyroidism, a condition characterized by an overactive thyroid gland producing too much thyroid hormone, often leads to insomnia and fragmented sleep. The heightened metabolic state and increased energy levels can make it difficult to fall asleep and stay asleep. Individuals with hyperthyroidism may experience racing thoughts and a general feeling of restlessness that interferes with relaxation and sleep onset.Common sleep symptoms associated with hyperthyroidism include:
- Insomnia, difficulty falling asleep
- Frequent awakenings during the night
- Restless sleep
- Increased heart rate and palpitations, which can disrupt sleep
- Anxiety and nervousness that interfere with sleep
- Night sweats
Importance of Balanced Thyroid Function for Restorative Sleep
Maintaining balanced thyroid hormone levels is crucial for ensuring the body can effectively regulate its sleep-wake cycles and achieve restorative sleep. When thyroid function is within the optimal range, it supports the proper functioning of the brain regions and neurotransmitter systems that govern sleep. This balance allows for efficient transitions between sleep stages, adequate time in deep sleep and REM sleep, and a natural feeling of wakefulness during the day.
A well-functioning thyroid gland is a cornerstone of healthy sleep architecture, enabling the body to undergo essential repair and rejuvenation processes during the night.
Key Hormones Influencing Sleep: Growth Hormone
Growth hormone (GH), often associated with childhood development and physical maturation, plays a significant role in adult physiology, including sleep regulation and repair processes. Its secretion is intricately linked to the sleep-wake cycle, particularly during specific stages of sleep. Understanding this connection is vital for appreciating the multifaceted impact of sleep on overall health and well-being.The release of growth hormone is not constant throughout the day but exhibits a distinct pulsatile pattern, with the most substantial surge occurring during the initial hours of sleep.
This nocturnal release is predominantly tied to deep sleep, also known as slow-wave sleep (SWS). This stage of sleep is characterized by slow brain wave activity and is considered the most restorative phase of sleep.
Growth Hormone Release and Deep Sleep Association
Growth hormone secretion is strongly correlated with the presence and depth of slow-wave sleep. During the first few hours of the night, as an individual transitions into deeper sleep stages, the pituitary gland releases pulses of GH. This timing suggests a coordinated effort between the brain’s sleep centers and the endocrine system to optimize the body’s regenerative processes during its most vulnerable and least active period.
The majority of daily growth hormone release occurs during slow-wave sleep.
This phenomenon highlights the importance of achieving sufficient amounts of deep sleep for maintaining optimal GH levels. The quality and duration of sleep directly influence the efficiency of this crucial hormonal release.
Adequate Deep Sleep for Optimal Growth Hormone Secretion
Sufficient deep sleep is a prerequisite for the body to effectively produce and release adequate amounts of growth hormone. During SWS, the body is in a state of reduced metabolic activity, allowing resources to be directed towards cellular repair, tissue regeneration, muscle growth, and bone development. These processes are all stimulated and facilitated by the release of growth hormone. Therefore, prioritizing sleep hygiene and ensuring consistent, restorative sleep is essential for supporting these vital functions, even in adulthood.
Consequences of Insufficient Sleep on Growth Hormone Production
Chronic sleep deprivation or consistently poor sleep quality can significantly disrupt the natural nocturnal release pattern of growth hormone. When deep sleep is compromised, the amplitude and frequency of GH pulses can be reduced. This diminished secretion can have several potential consequences, impacting various bodily functions:
- Reduced capacity for tissue repair and muscle recovery, potentially affecting athletic performance and overall physical resilience.
- Impaired metabolic regulation, which may contribute to increased body fat and a higher risk of developing metabolic disorders over time.
- Potential negative effects on bone density and strength, particularly concerning for long-term skeletal health.
- A general feeling of reduced vitality and increased susceptibility to illness due to compromised immune function, which is also influenced by adequate sleep and GH.
Hormonal Imbalances and Sleep Disorders
The intricate dance of hormones is fundamental to maintaining our body’s equilibrium, and disruptions in this delicate balance can significantly impact our sleep quality. When hormonal levels fluctuate beyond their optimal ranges, a cascade of physiological changes can occur, leading to various sleep disturbances. Understanding these connections is crucial for identifying the root causes of persistent sleep issues and seeking appropriate interventions.Several common sleep disorders are intrinsically linked to specific hormonal imbalances, highlighting the profound influence of our endocrine system on our nocturnal rest.
These imbalances can affect the natural sleep-wake cycle, increase arousal, or impair the restorative processes that occur during sleep.
Sleep Disorders Associated with Hormonal Imbalances
A variety of sleep disorders can manifest or be exacerbated by hormonal dysregulation. Recognizing these associations allows for a more targeted approach to diagnosis and treatment.
- Insomnia: This is a prevalent sleep disorder characterized by difficulty falling asleep, staying asleep, or experiencing non-restorative sleep. Hormonal imbalances, particularly those involving cortisol, thyroid hormones, and sex hormones, are frequently implicated.
- Sleep Apnea: While not solely a hormonal disorder, hormonal changes can contribute to its development or severity. For instance, hormonal shifts in menopause can lead to weight gain and changes in airway tissues, increasing the risk of obstructive sleep apnea.
- Restless Legs Syndrome (RLS): This neurological disorder causing an irresistible urge to move the legs can be linked to iron deficiency, which itself can be influenced by hormonal factors, and is sometimes observed during pregnancy due to hormonal shifts.
- Circadian Rhythm Sleep-Wake Disorders: These disorders involve a misalignment between the body’s internal clock and the external environment. Hormones like melatonin and cortisol play a central role in regulating the circadian rhythm, and imbalances can disrupt this crucial timing mechanism.
Mechanisms of Hormonal Disruption in Sleep
Specific hormonal imbalances can disrupt sleep through various physiological pathways, affecting the brain’s sleep-regulating centers and the body’s overall state of arousal.
Polycystic Ovary Syndrome (PCOS) and Sleep Disruption
PCOS is a common endocrine disorder characterized by irregular periods, excess androgens, and polycystic ovaries. The hormonal fluctuations associated with PCOS, particularly elevated androgens and insulin resistance, can significantly impact sleep.
- Androgen Excess: High levels of androgens can increase daytime sleepiness and contribute to fragmented sleep. They may also interfere with the production and signaling of neurotransmitters involved in sleep regulation.
- Insulin Resistance: A common feature of PCOS, insulin resistance can lead to fluctuations in blood sugar levels, which can cause awakenings during the night. It can also affect the production of other hormones that influence sleep.
- Associated Conditions: PCOS is often linked with conditions like sleep apnea and anxiety, both of which can further exacerbate sleep problems.
Adrenal Fatigue and Sleep Disturbances
The concept of “adrenal fatigue” or adrenal insufficiency, while not a universally accepted medical diagnosis in all its proposed forms, refers to a state where the adrenal glands are believed to be unable to produce adequate levels of hormones like cortisol in response to stress.
- Cortisol Dysregulation: In states described as adrenal fatigue, the typical diurnal pattern of cortisol (high in the morning, low at night) can be disrupted. This can lead to elevated cortisol levels at night, interfering with the ability to fall asleep and stay asleep, and low cortisol levels in the morning, contributing to fatigue and difficulty waking.
- Stress Response: The adrenal glands are central to the body’s stress response. Chronic stress can lead to prolonged activation of the adrenal glands, eventually contributing to their perceived inability to function optimally, thereby impacting sleep-wake cycles.
Age-Related Hormonal Changes and Sleep
As individuals age, natural hormonal shifts occur, which can significantly alter sleep patterns and contribute to sleep disorders.
Menopause and Sleep Issues
Menopause, the cessation of menstruation in women, is marked by a significant decline in estrogen and progesterone levels. These hormonal changes are strongly linked to sleep disturbances.
- Hot Flashes and Night Sweats: The dramatic drop in estrogen can trigger vasomotor symptoms like hot flashes and night sweats, which can cause awakenings and disrupt sleep architecture.
- Changes in Sleep Architecture: Reduced estrogen and progesterone can lead to a decrease in slow-wave sleep (deep sleep) and an increase in lighter stages of sleep, resulting in less restorative sleep.
- Mood Changes: Hormonal shifts can also influence mood, leading to increased anxiety or depression, which are common co-occurring conditions with insomnia in menopausal women.
Lifestyle Factors Exacerbating Hormonal Influences on Sleep
While hormonal imbalances are a primary driver of sleep disturbances, lifestyle factors can significantly amplify their effects, creating a challenging cycle for individuals.
- Diet: Poor dietary choices, such as excessive consumption of caffeine and alcohol, or irregular meal patterns, can disrupt blood sugar levels and further strain the endocrine system, negatively impacting sleep. For instance, a diet high in processed sugars can exacerbate insulin resistance, a common issue in PCOS.
- Exercise: While regular exercise is beneficial, exercising too close to bedtime can increase arousal and interfere with sleep onset. Conversely, a lack of physical activity can contribute to weight gain, which can worsen sleep apnea and hormonal imbalances.
- Stress Management: Chronic psychological stress leads to elevated cortisol levels, which directly interferes with sleep. Ineffective stress management techniques can prolong this hormonal dysregulation.
- Screen Time: Exposure to blue light from electronic devices before bed can suppress melatonin production, a hormone crucial for signaling sleepiness, thereby disrupting the natural sleep-wake cycle.
Lifestyle Factors and Hormone-Sleep Connection
The intricate relationship between our lifestyle choices and hormonal regulation significantly influences sleep quality and overall well-being. Factors such as diet, exercise, and stress management play a crucial role in maintaining the delicate balance of hormones that govern our sleep-wake cycles. Understanding these connections empowers us to make informed decisions that promote better sleep and hormonal health.
Diet and Nutrition’s Impact on Hormones and Sleep
The foods we consume directly affect the production and regulation of various hormones, including those essential for sleep. A balanced diet rich in essential nutrients supports the endocrine system’s optimal functioning, while certain dietary patterns can disrupt hormonal balance and negatively impact sleep.Here are key aspects of diet and nutrition influencing hormone-sleep connection:
- Macronutrient Balance: Adequate intake of proteins, healthy fats, and complex carbohydrates is vital for hormone synthesis and stability. For instance, insufficient protein can impair the production of neurotransmitters like serotonin, which is a precursor to melatonin, the sleep hormone.
- Micronutrient Sufficiency: Vitamins and minerals act as cofactors in numerous hormonal pathways. Magnesium, for example, plays a role in melatonin production and muscle relaxation, while B vitamins are crucial for energy metabolism and neurotransmitter synthesis. Deficiencies in these can lead to sleep disturbances.
- Blood Sugar Regulation: Fluctuations in blood sugar levels can trigger hormonal responses that interfere with sleep. High intake of refined sugars and processed foods can lead to rapid spikes and crashes in blood glucose, prompting the release of cortisol and adrenaline, which promote wakefulness. Conversely, maintaining stable blood sugar through balanced meals and snacks helps support consistent sleep.
- Gut Health: The gut microbiome communicates with the brain through the gut-brain axis, influencing the production of neurotransmitters and hormones. A diet rich in fiber and fermented foods supports a healthy gut, which can positively impact mood and sleep regulation.
- Specific Foods and Beverages: Caffeine and alcohol can disrupt sleep architecture by interfering with melatonin production and sleep cycles. Consuming these close to bedtime is generally advised against. Conversely, foods containing tryptophan, like turkey and dairy, can promote relaxation and sleep.
Exercise Timing and Intensity for Hormone Regulation and Sleep
Physical activity is a powerful modulator of hormonal responses, and its timing and intensity are critical for optimizing sleep. Regular exercise can improve sleep quality by influencing the production of hormones like cortisol and endorphins, but exercising too close to bedtime or engaging in excessively strenuous activity can have the opposite effect.The following points highlight the role of exercise in the hormone-sleep connection:
- Cortisol Regulation: Exercise, particularly moderate-intensity aerobic activity, can help regulate the body’s natural cortisol rhythm. Exercising earlier in the day can help lower elevated cortisol levels that may have accumulated due to daily stressors, promoting relaxation in the evening. Intense exercise late in the day, however, can elevate cortisol and adrenaline, making it harder to fall asleep.
- Endorphin Release: Exercise stimulates the release of endorphins, which have mood-boosting and stress-reducing effects. While beneficial for overall well-being, the timing of this release is important. Exercise-induced endorphin release can promote a sense of calm and fatigue, conducive to sleep, if performed several hours before bedtime.
- Body Temperature Regulation: Exercise temporarily raises body temperature. A slight drop in body temperature is a signal for sleep onset. Engaging in exercise earlier in the day allows the body temperature to return to its baseline and then cool down, facilitating sleep. Late-night exercise can prevent this natural cooling process.
- Growth Hormone and Sleep: Exercise, especially resistance training, stimulates the release of growth hormone, which is predominantly released during deep sleep. Therefore, regular exercise can indirectly enhance sleep quality by promoting the conditions for optimal growth hormone secretion during sleep.
- Consistency and Moderation: Consistent exercise routines, rather than sporadic intense bursts, are more effective for long-term hormonal balance and sleep improvement. Finding a balance in intensity that challenges the body without overstimulating it before sleep is key.
Chronic Stress and the Endocrine System’s Impact on Sleep
Chronic stress is a significant disruptor of the endocrine system, leading to prolonged activation of the “fight-or-flight” response and dysregulation of key hormones, profoundly affecting sleep patterns. The continuous exposure to stress hormones like cortisol can create a state of hyperarousal that makes falling asleep and staying asleep challenging.The effects of chronic stress on the endocrine system and sleep are multifaceted:
- Cortisol Dysregulation: Under chronic stress, the hypothalamic-pituitary-adrenal (HPA) axis remains persistently activated, leading to elevated cortisol levels, particularly in the evening when they should be declining. This elevated cortisol interferes with melatonin production and promotes wakefulness, contributing to insomnia and fragmented sleep.
- Adrenaline and Noradrenaline Release: Stress hormones like adrenaline and noradrenaline are released to prepare the body for immediate action. Chronic stress means these hormones are frequently elevated, leading to a heightened state of alertness and anxiety that makes it difficult for the body and mind to relax and transition into sleep.
- Impact on Other Hormones: Chronic stress can also indirectly affect other hormones involved in sleep, such as sex hormones and thyroid hormones, by disrupting the overall endocrine balance. For instance, prolonged high cortisol can suppress reproductive hormone production.
- Sleep Architecture Disruption: The hormonal imbalances caused by chronic stress can alter the normal progression through sleep stages. Individuals may experience less deep sleep (slow-wave sleep) and more light sleep, leading to a feeling of unrefreshing sleep, even if the total duration seems adequate.
- Learned Helplessness and Sleep: Over time, the persistent struggle to sleep due to stress can lead to anxiety about sleep itself, creating a vicious cycle. This psychological component further exacerbates the physiological hormonal disruptions.
Establishing Healthy Sleep Hygiene Practices for Hormonal Balance
Implementing robust sleep hygiene practices is fundamental to supporting hormonal balance and improving sleep quality. These practices create an environment and routine conducive to the body’s natural sleep-wake cycles and hormonal regulation.Here are essential sleep hygiene practices that support hormonal balance:
- Consistent Sleep Schedule: Going to bed and waking up around the same time every day, even on weekends, helps regulate the body’s internal clock (circadian rhythm). This consistency reinforces the natural release patterns of hormones like melatonin and cortisol.
- Optimizing the Sleep Environment: Ensure your bedroom is dark, quiet, and cool. Darkness is crucial for melatonin production, while a cool temperature aids in the body’s natural temperature drop associated with sleep onset.
- Limiting Exposure to Blue Light: The blue light emitted from electronic devices (phones, tablets, computers) can suppress melatonin production. Avoiding these devices for at least an hour before bedtime signals to the brain that it’s time to wind down.
- Mindful Evening Routine: Develop a relaxing pre-sleep routine. This could include activities like reading a book, taking a warm bath, or gentle stretching. These activities help reduce stress hormones and prepare the body for sleep.
- Dietary Considerations Before Bed: Avoid heavy meals, caffeine, and alcohol close to bedtime. A light, sleep-promoting snack, if needed, can help maintain stable blood sugar levels overnight.
- Regular Physical Activity (Timed Appropriately): Engage in regular exercise, but aim to complete moderate to vigorous workouts at least a few hours before bedtime to allow for adequate recovery and cooling down.
- Stress Management Techniques: Incorporate daily stress-reducing practices such as meditation, deep breathing exercises, or journaling. These techniques help to mitigate the negative impact of chronic stress on the endocrine system.
- Limit Napping: While short naps can be beneficial, long or late-afternoon naps can disrupt nighttime sleep by interfering with the body’s sleep drive and hormonal cues.
Natural Approaches to Support Hormonal Sleep Regulation
Understanding the intricate dance between hormones and sleep is the first step towards achieving restful nights. Fortunately, nature offers a wealth of remedies and practices that can gently guide your body back into hormonal balance, promoting deeper and more restorative sleep. This section explores actionable strategies, from daily routines to specific supplements, that can empower you to harness these natural pathways for improved sleep quality.Harnessing natural approaches involves a holistic perspective, recognizing that our daily habits, environment, and even what we consume can significantly impact our hormonal equilibrium and, consequently, our sleep.
By integrating these practices, we can create a supportive ecosystem for our bodies to naturally regulate sleep-inducing hormones and minimize those that disrupt it.
Natural Remedies and Practices for Hormone Regulation and Sleep
Several natural remedies and lifestyle practices have been identified to help regulate hormones that influence sleep. These interventions focus on reducing stress, promoting relaxation, and supporting the body’s natural circadian rhythms.
- Consistent Sleep Schedule: Adhering to a regular bedtime and wake-up time, even on weekends, helps to synchronize the body’s internal clock (circadian rhythm), which is crucial for regulating hormones like melatonin and cortisol.
- Mindful Eating and Hydration: Avoiding heavy meals, caffeine, and alcohol close to bedtime can prevent digestive discomfort and stimulant effects that interfere with sleep. Staying adequately hydrated throughout the day, but limiting fluid intake before bed, also contributes to uninterrupted sleep.
- Regular Physical Activity: Engaging in moderate exercise most days of the week can improve sleep quality and help regulate stress hormones. However, intense workouts too close to bedtime may have an alerting effect for some individuals.
- Exposure to Natural Light: Spending time outdoors, especially in the morning, helps to set the body’s natural circadian rhythm, signaling wakefulness and influencing melatonin production later in the day.
- Herbal Teas: Certain herbal teas, such as chamomile, valerian root, and passionflower, have been traditionally used for their calming properties and ability to promote relaxation and sleep.
- Aromatherapy: The use of essential oils like lavender, bergamot, and ylang-ylang in diffusers or baths can create a calming atmosphere conducive to sleep.
- Mindfulness and Meditation: Regular practice of mindfulness and meditation can reduce stress and anxiety, thereby lowering cortisol levels and facilitating sleep onset.
Sample Daily Routine for Optimal Hormone Balance and Sleep
A structured daily routine can significantly contribute to balancing hormones that affect sleep. This sample routine integrates various natural approaches to support your body’s natural rhythms and promote restful sleep.
- Morning (Upon Waking):
- Expose yourself to bright natural light for at least 15-30 minutes to signal wakefulness and regulate your circadian rhythm.
- Engage in light physical activity, such as a short walk or stretching.
- Consume a balanced breakfast, focusing on protein and healthy fats.
- Midday:
- Continue to seek natural light exposure.
- Incorporate a brief mindfulness or breathing exercise to manage stress.
- Stay hydrated by drinking water throughout the day.
- Afternoon:
- Engage in moderate exercise if not done in the morning.
- Avoid large amounts of caffeine.
- Evening (2-3 Hours Before Bed):
- Consume a light, easily digestible dinner.
- Begin to wind down by dimming lights and reducing screen time.
- Consider a warm bath with Epsom salts or a few drops of lavender essential oil.
- Before Bed:
- Engage in a relaxing activity, such as reading a physical book, gentle stretching, or listening to calming music.
- Practice a short relaxation technique (detailed below).
- Ensure your bedroom is dark, quiet, and cool.
Relaxation Techniques for Stress Hormone Reduction and Sleep Onset
Stress hormones, particularly cortisol, can significantly interfere with the ability to fall asleep and stay asleep. Implementing specific relaxation techniques can effectively lower these hormone levels, paving the way for a more peaceful transition into sleep.
- Deep Breathing Exercises: Also known as diaphragmatic breathing, this technique involves slow, deep inhalations through the nose, allowing the abdomen to rise, followed by a slow exhalation through the mouth. This activates the parasympathetic nervous system, counteracting the “fight or flight” response. A common technique is the 4-7-8 method: inhale for a count of 4, hold for a count of 7, and exhale for a count of 8.
- Progressive Muscle Relaxation (PMR): This practice involves systematically tensing and then releasing different muscle groups in the body. By focusing on the physical sensations of tension and release, individuals can become more aware of bodily tension and learn to consciously relax it, which can reduce overall physiological arousal.
- Guided Imagery: This technique involves using one’s imagination to create peaceful and calming mental images or scenarios. By focusing on these positive and tranquil mental landscapes, individuals can distract themselves from stressful thoughts and promote a sense of calm.
- Mindful Body Scan: This practice involves bringing gentle, non-judgmental awareness to different parts of the body, noticing any sensations without trying to change them. This can help to release physical tension and promote a sense of grounding and relaxation.
Benefits of Specific Supplements for Hormone and Sleep Support
While lifestyle changes are foundational, certain supplements can offer targeted support for hormonal balance and improved sleep. It is always advisable to consult with a healthcare professional before starting any new supplement regimen, especially if you have underlying health conditions or are taking medications.
Magnesium
Magnesium is a mineral involved in over 300 biochemical reactions in the body, including those that regulate neurotransmitters and hormones essential for sleep. It plays a role in the regulation of melatonin, the sleep hormone, and can help to calm the nervous system by blocking the activity of excitatory neurotransmitters. Magnesium deficiency has been linked to sleep disturbances, insomnia, and restless legs syndrome.
Supplementation may help improve sleep quality, reduce the time it takes to fall asleep, and decrease nighttime awakenings.
Magnesium is crucial for GABA receptor function, which promotes relaxation and sleep.
Adaptogens
Adaptogens are a class of herbs and mushrooms that are believed to help the body adapt to stress and promote homeostasis. They work by modulating the stress response system, particularly the hypothalamic-pituitary-adrenal (HPA) axis, which is central to cortisol regulation. By helping to balance cortisol levels, adaptogens can reduce the stimulatory effects of stress that often disrupt sleep.
- Ashwagandha (Withania somnifera): This well-researched adaptogen has demonstrated an ability to reduce cortisol levels, improve sleep quality, and alleviate symptoms of anxiety and stress. Studies suggest it can help reduce the time it takes to fall asleep and improve overall sleep duration.
- Rhodiola Rosea: While often used for energy and focus, Rhodiola can also help to normalize the stress response, preventing burnout and improving resilience. By moderating the body’s reaction to stress, it can indirectly support better sleep by reducing nighttime awakenings caused by stress.
- Holy Basil (Tulsi): Known for its adaptogenic and antioxidant properties, Holy Basil has been used in Ayurvedic medicine to combat stress and promote well-being. It can help to calm the mind and body, making it easier to fall asleep.
When to Seek Professional Guidance

Understanding the intricate relationship between hormones and sleep is a journey, and while self-education is valuable, recognizing when to enlist professional help is crucial for effective management and well-being. Persistent sleep disturbances or suspected hormonal imbalances warrant a consultation with a healthcare provider to ensure accurate diagnosis and appropriate intervention.Identifying specific signs and symptoms is the first step in determining the need for professional guidance.
These indicators can range from noticeable changes in sleep patterns to broader physical and emotional alterations that might be linked to hormonal fluctuations.
Recognizing Signs and Symptoms Indicating Professional Consultation
Several key indicators suggest that a conversation with a healthcare professional about your sleep and hormone health is advisable. These signs often point to underlying issues that require expert assessment and management.
- Persistent insomnia or difficulty falling asleep, even with good sleep hygiene practices.
- Excessive daytime sleepiness that interferes with daily activities and cognitive function.
- Frequent awakenings during the night, accompanied by difficulty returning to sleep.
- Noticeable changes in mood, such as increased irritability, anxiety, or depression, that coincide with sleep disturbances.
- Unexplained weight gain or loss that is not attributable to diet or exercise.
- Significant changes in energy levels, including chronic fatigue.
- Irregular menstrual cycles or the onset of menopausal symptoms in women.
- Symptoms related to low testosterone in men, such as decreased libido or muscle mass.
- Hot flashes or night sweats that disrupt sleep.
- Digestive issues or changes in appetite that accompany sleep problems.
Medical Evaluations for Diagnosing Hormonal Imbalances Affecting Sleep
When you consult a healthcare professional, they will employ various diagnostic tools to pinpoint the cause of your sleep and hormone-related issues. These evaluations are designed to provide a comprehensive understanding of your hormonal status and its impact on your sleep.
The goal of medical evaluations is to move beyond symptom observation to objective measurement of hormone levels and related physiological functions.
A typical diagnostic process may involve:
- Detailed Medical History and Physical Examination: The physician will gather information about your symptoms, lifestyle, diet, medications, and family history. A physical exam can reveal signs related to hormonal imbalances.
- Blood Tests: These are the cornerstone of hormonal assessment. Specific blood tests can measure levels of key hormones such as cortisol, melatonin, thyroid hormones (TSH, T3, T4), estrogen, progesterone, testosterone, and growth hormone. Tests may be conducted at specific times of the day or menstrual cycle to accurately reflect hormone fluctuations.
- Saliva Tests: For certain hormones, particularly cortisol and melatonin, saliva tests can offer a convenient way to track diurnal (daily) variations in hormone levels, which are critical for understanding sleep-wake cycles.
- Urine Tests: These can be used to measure hormone metabolites, providing a broader picture of hormone production and breakdown over a 24-hour period.
- Sleep Studies (Polysomnography): If sleep apnea or other primary sleep disorders are suspected, a sleep study may be recommended. This non-invasive test monitors brain waves, oxygen levels, heart rate, breathing, and body movements during sleep.
- Imaging Studies: In some cases, imaging tests like ultrasounds or MRIs might be used to examine endocrine glands (e.g., thyroid, adrenal glands, pituitary gland) for abnormalities.
The Role of Medical Professionals in Developing Personalized Treatment Plans
Once a diagnosis is established, medical professionals play a vital role in creating tailored treatment strategies that address both the hormonal imbalance and the resulting sleep disturbances. This personalized approach ensures that interventions are effective and safe for the individual.The development of a treatment plan typically involves a collaborative effort between the patient and their healthcare provider. This plan may incorporate a combination of medical and lifestyle interventions.
- Hormone Replacement Therapy (HRT): If a significant deficiency or excess of a particular hormone is identified, HRT may be prescribed. This could involve bioidentical hormones or synthetic versions, carefully dosed to restore balance. For example, individuals with low melatonin might benefit from melatonin supplementation, while those with adrenal fatigue might receive guidance on cortisol management.
- Medication Management: Depending on the underlying cause, medications might be prescribed to manage specific hormonal conditions or to directly address sleep issues, such as sleep aids or medications to regulate circadian rhythms.
- Lifestyle Modifications: Medical professionals will guide you on essential lifestyle changes that support hormonal balance and improve sleep. This includes:
- Dietary adjustments to optimize nutrient intake and support hormone production.
- Stress management techniques, such as mindfulness, meditation, or yoga, to help regulate cortisol levels.
- Establishing a consistent sleep schedule and optimizing sleep hygiene.
- Incorporating regular physical activity, while being mindful of timing to avoid disrupting sleep.
- Nutritional Counseling: Guidance on specific vitamins and minerals that play a role in hormone synthesis and function, such as vitamin D, magnesium, and B vitamins.
- Referral to Specialists: In complex cases, a referral to an endocrinologist (hormone specialist), a sleep specialist, or a mental health professional may be necessary to provide comprehensive care.
Outcome Summary

In concluding our journey through the complex interplay of hormones and sleep, we’ve uncovered the essential mechanisms that govern our nightly rest and the profound impact hormonal fluctuations can have. By recognizing the roles of key hormones and understanding how lifestyle factors can influence them, we are empowered to make informed choices that foster better sleep and overall well-being. This knowledge serves as a foundation for seeking balance and promoting restorative sleep.