As How to Sleep Comfortably with Chronic Back Pain takes center stage, this opening passage beckons readers into a world crafted with good knowledge, ensuring a reading experience that is both absorbing and distinctly original. We understand that chronic back pain can significantly disrupt your sleep, turning what should be a period of rest and recovery into a nightly struggle.
This comprehensive guide is designed to empower you with the understanding and practical strategies needed to find true comfort and achieve restorative sleep, even with persistent back discomfort.
This exploration delves into the intricate relationship between chronic back pain and sleep disruption, examining how various types of pain affect your sleeping positions and the physiological consequences on sleep quality. We will navigate the cycle of pain and poor sleep, offering insights into optimizing your sleep environment, selecting supportive mattresses and pillows, and discovering the most beneficial sleeping positions.
Furthermore, we will explore the integration of supportive aids and gentle techniques, alongside crucial lifestyle adjustments, to foster better sleep and reduce pain. Finally, we will guide you on when and how to seek professional help for persistent issues.
Understanding Back Pain and Sleep Disruption
Chronic back pain can significantly interfere with restful sleep, creating a challenging cycle that impacts overall well-being. Understanding the intricate relationship between back pain and sleep is the first crucial step toward finding effective strategies for comfort. This section will explore the common origins of back pain that disrupt sleep, how different pain locations influence sleeping positions, the physiological consequences of chronic pain on sleep, and the self-perpetuating nature of the pain-sleep cycle.The persistent discomfort associated with chronic back pain often makes it difficult to find a comfortable sleeping position, leading to frequent awakenings and reduced sleep efficiency.
This disruption not only affects physical recovery but also has profound implications for mental health and daily functioning. By delving into the specific ways back pain impacts sleep, we can better equip ourselves with knowledge to mitigate its effects.
Common Causes of Chronic Back Pain Affecting Sleep
Chronic back pain, the kind that lingers for months or even years, can stem from a variety of underlying issues. These conditions often intensify during periods of rest, making sleep a significant challenge. Understanding these causes is vital for developing targeted pain management strategies that promote better sleep.Common culprits include:
- Degenerative Disc Disease: As we age, the intervertebral discs can lose hydration and shrink, leading to reduced cushioning between vertebrae. This can cause stiffness and pain, particularly when lying down for extended periods.
- Herniated or Bulging Discs: When the soft inner material of a spinal disc pushes through its outer layer, it can press on nearby nerves, causing sharp, radiating pain that is often aggravated by certain positions.
- Osteoarthritis: This condition affects the joints in the spine, leading to inflammation and stiffness. The cartilage that cushions the joints wears down, resulting in bone-on-bone friction and pain, especially during inactivity.
- Sciatica: This is not a condition itself but a symptom, typically caused by a herniated disc or spinal stenosis, characterized by pain that radiates along the path of the sciatic nerve, often from the lower back down the leg. This can make it difficult to find a comfortable side or back sleeping position.
- Muscle Strains and Ligament Sprains: While often acute, chronic or recurring strains and sprains can lead to persistent inflammation and pain, especially in muscles that are tense from prolonged sitting or poor posture.
- Spinal Stenosis: This condition involves the narrowing of the spinal canal, which can put pressure on the spinal cord and nerves. Pain and numbness are often worse when lying flat or in positions that compress the spine.
- Fibromyalgia: This widespread musculoskeletal pain condition often includes fatigue and sleep disturbances. While not solely a back pain issue, it frequently manifests with significant back discomfort and generalized body aches that disrupt sleep.
Influence of Back Pain Location on Sleep Positions
The specific area of the back experiencing pain plays a significant role in determining which sleeping positions are most tolerable and which exacerbate discomfort. Understanding these correlations can guide individuals in experimenting with different sleeping postures to find relief.For individuals experiencing pain in different regions of the spine, certain positions are often more problematic:
- Lumbar (Lower Back) Pain: This is the most common type of back pain.
- Sleeping on the stomach is generally discouraged as it flattens the natural curve of the spine, leading to strain.
- Sleeping on the back can be tolerable if a pillow is placed under the knees to maintain the natural lumbar curve. Without this support, the lower back can arch unnaturally.
- Sleeping on the side, with a pillow between the knees, is often recommended to keep the hips, pelvis, and spine aligned. This prevents the upper leg from pulling the spine out of alignment.
- Thoracic (Mid-Back) Pain: Pain in this region can be linked to poor posture, spinal arthritis, or rib issues.
- Sleeping on the stomach can put pressure on the rib cage and thoracic spine.
- Sleeping on the back can be comfortable for some, but may require a supportive pillow for the head and neck to prevent strain.
- Sleeping on the side might be comfortable, but requires careful pillow placement to support the torso and prevent twisting.
- Cervical (Neck) Pain: While technically part of the spine, cervical pain often affects the entire back due to its connection.
- The position of the head and neck is paramount. A supportive pillow that maintains the natural curve of the neck is essential, regardless of whether one sleeps on their back or side.
- Sleeping on the stomach is generally ill-advised as it forces the neck into an unnatural, twisted position for prolonged periods.
Physiological Effects of Chronic Back Pain on Sleep Quality and Duration
Chronic back pain doesn’t just cause physical discomfort; it triggers a cascade of physiological responses that directly impair sleep quality and reduce its overall duration. These effects can significantly impact an individual’s ability to achieve restorative sleep, leading to daytime fatigue and other health issues.The physiological disruptions include:
- Increased Muscle Tension: The body’s natural response to pain is to tense the surrounding muscles, creating a protective guarding mechanism. This chronic tension makes it difficult to relax into sleep and can lead to stiffness upon waking.
- Elevated Stress Hormones: Pain is a stressor, and chronic pain can lead to persistently elevated levels of cortisol and adrenaline. These hormones are designed to promote alertness and can interfere with the body’s natural sleep-wake cycle, making it harder to fall asleep and stay asleep.
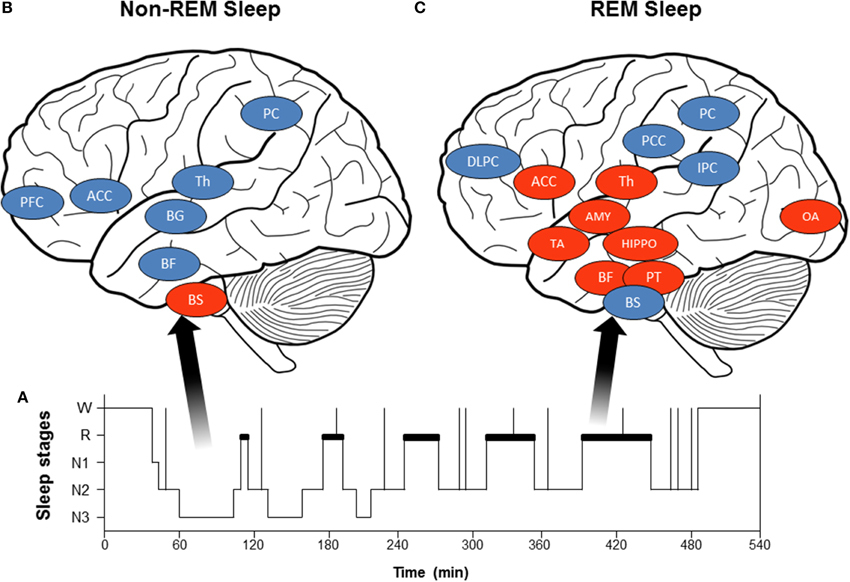
- Fragmented Sleep: Individuals with chronic back pain often experience frequent micro-arousals, where they briefly wake up without full consciousness. These awakenings disrupt the normal progression through sleep stages, particularly deep sleep and REM sleep, which are crucial for physical and mental restoration.
- Reduced Sleep Efficiency: Sleep efficiency is the percentage of time spent asleep while in bed. Chronic pain often leads to longer latency to sleep onset (taking longer to fall asleep) and more time awake during the night, thus reducing overall sleep efficiency.
- Inflammatory Responses: Chronic pain, especially when related to inflammatory conditions like arthritis, can be associated with increased systemic inflammation. This inflammation can disrupt sleep-regulating neurotransmitters and pathways, further contributing to poor sleep.
- Altered Sleep Architecture: Studies have shown that chronic pain can alter the normal pattern of sleep stages. This can mean spending less time in the deeper, more restorative stages of sleep and more time in lighter sleep stages, leading to a feeling of not being well-rested.
The Cycle of Pain and Poor Sleep
The relationship between chronic back pain and poor sleep is often described as a vicious cycle, where each condition exacerbates the other, creating a persistent loop that is difficult to break. Understanding this cycle is fundamental to developing effective strategies for managing both pain and sleep disturbances.The cycle typically unfolds as follows:
- Pain Interferes with Sleep: When experiencing chronic back pain, it becomes difficult to find a comfortable sleeping position. This leads to frequent awakenings, discomfort, and an inability to fall into deep, restorative sleep.
- Poor Sleep Worsens Pain Perception: Lack of adequate sleep significantly impacts the body’s ability to manage pain. Sleep deprivation lowers pain thresholds, making individuals more sensitive to discomfort. Furthermore, insufficient sleep can increase inflammation, which can directly contribute to or worsen back pain.
- Increased Muscle Tension and Fatigue: When sleep is poor, muscles do not get adequate time to repair and recover. This can lead to increased muscle tension and fatigue, which in turn can exacerbate back pain. The body may also adopt more guarded postures to cope with pain and fatigue, further contributing to discomfort.
- Psychological Distress: The combination of chronic pain and sleep deprivation can lead to increased stress, anxiety, and depression. These psychological factors can further amplify pain perception and make it even harder to relax and fall asleep, thus completing the cycle.
This interconnectedness means that addressing one aspect of the cycle often has a positive impact on the other. For instance, finding ways to improve sleep can lead to a reduction in pain sensitivity, and effectively managing pain can allow for more restful sleep.
“The interdependency of pain and sleep creates a formidable challenge, where improving one often necessitates addressing the other in tandem.”
Optimizing Sleep Environment for Comfort
Creating a sleep sanctuary is paramount for anyone experiencing chronic back pain. Your bedroom environment plays a significant role in either exacerbating or alleviating discomfort, directly impacting your ability to achieve restful sleep. By carefully considering and adjusting key elements, you can transform your bedroom into a haven that supports spinal health and promotes deep, restorative sleep.This section will delve into the essential components of an optimized sleep environment, focusing on how each element can be tailored to benefit individuals with chronic back pain.
We will explore the ideal conditions for temperature, lighting, and sound, and then focus on the critical role of your mattress and pillows in ensuring proper spinal alignment.
Essential Elements for a Sleep-Friendly Bedroom
A truly sleep-friendly bedroom is a harmonious blend of sensory inputs designed to signal to your body that it’s time to rest. For individuals managing chronic back pain, these elements become even more crucial as they can directly influence muscle tension and joint comfort.Here are the fundamental elements to consider when optimizing your sleep space:
- Comfortable Mattress and Pillows: The foundation of good sleep, these must provide adequate support and cushioning.
- Appropriate Temperature: A cool room generally promotes better sleep quality.
- Controlled Lighting: Darkness is key for melatonin production, the sleep hormone.
- Minimal Noise: A quiet environment reduces awakenings and promotes deeper sleep cycles.
- Clean and Clutter-Free Space: A tidy room can reduce mental stress, contributing to a calmer state conducive to sleep.
- Comfortable Bedding: Breathable fabrics that feel good against the skin enhance overall comfort.
- Absence of Electronics: Minimizing blue light exposure from screens before bed is vital.
Ideal Bedroom Temperature, Lighting, and Sound Levels
The physiological responses to environmental cues are powerful. For individuals with chronic back pain, optimizing these sensory inputs can significantly contribute to pain reduction and improved sleep onset and maintenance.The ideal conditions for sleep are as follows:
- Temperature: A study published in the Journal of Clinical Sleep Medicine suggests that the optimal room temperature for sleep is between 60-67 degrees Fahrenheit (15.6-19.4 degrees Celsius). This slight coolness helps lower your core body temperature, which is a natural signal for sleep initiation. For back pain sufferers, a cooler environment can also help reduce muscle inflammation and stiffness.
- Lighting: Complete darkness is essential for the body to produce melatonin, a hormone that regulates sleep-wake cycles. Even small amounts of light can disrupt this process. Blackout curtains or an eye mask can be highly effective in achieving a dark environment. Avoid using bright lights in the bedroom in the hours leading up to sleep. Dim, warm-toned lighting is preferable if you need to move around.
- Sound Levels: Excessive noise can fragment sleep, leading to more frequent awakenings and reduced time spent in deep sleep stages. Aim for a quiet environment. If complete silence is not achievable, consider using a white noise machine or earplugs. White noise can mask sudden, disruptive sounds and create a consistent, calming auditory backdrop.
Benefits of a Supportive Mattress and Pillow for Spinal Alignment
The cornerstone of comfortable sleep for individuals with chronic back pain lies in the support provided by their mattress and pillows. These items are not merely for comfort; they are crucial for maintaining proper spinal alignment throughout the night. Misalignment can put undue stress on muscles, ligaments, and discs, leading to increased pain and stiffness upon waking.A supportive mattress and pillow work synergistically to:
- Maintain Natural Spinal Curvature: They should cradle your body’s contours, ensuring that your spine rests in its natural “S” shape, whether you sleep on your back, side, or stomach.
- Distribute Body Weight Evenly: This prevents pressure points that can cause discomfort and exacerbate pain in specific areas of your back.
- Reduce Motion Transfer: For those who share a bed, a mattress that minimizes the transfer of movement can prevent disturbances from a partner’s tossing and turning.
- Promote Muscle Relaxation: When the spine is properly aligned, the muscles supporting it can relax more effectively, reducing tension and fatigue.
- Prevent Stiffness: By avoiding awkward sleeping positions and pressure points, you can wake up feeling less stiff and more mobile.
Types of Mattresses and Pillows Best Suited for Various Back Pain Conditions
Selecting the right mattress and pillow is a highly individualized process, especially when dealing with chronic back pain. Different types of back pain may respond better to specific materials and firmness levels. Understanding these nuances can help you make an informed decision.Here is a guide to mattress and pillow types suitable for common back pain conditions:
Mattresses
The choice of mattress material and firmness is critical. Generally, a medium-firm to firm mattress is recommended for back pain sufferers as it offers a good balance of support and cushioning.
- Memory Foam Mattresses: These contour to your body, providing excellent pressure relief and support. They are particularly good for side sleepers and those with hip or shoulder pain, as they can reduce pressure points. However, some individuals may find them too hot, and very soft memory foam might not offer enough support for severe back pain. Look for higher-density memory foam for better durability and support.
- Innerspring Mattresses: These offer a traditional feel with coils providing support. Pocketed coils, where each coil is individually wrapped, offer better motion isolation and contouring than traditional interconnected coils. A medium-firm innerspring mattress with a comfortable pillow-top can be a good option for back sleepers.
- Latex Mattresses: Made from natural or synthetic latex, these offer a responsive, buoyant feel. They are durable, breathable, and provide excellent support and pressure relief. Natural latex is a more eco-friendly option. Latex mattresses are suitable for various sleeping positions and can be a good choice for those with sensitive backs.
- Hybrid Mattresses: These combine the support of an innerspring system with the contouring comfort of foam layers (memory foam or latex). They often provide the best of both worlds, offering robust support and excellent pressure relief. They are a versatile choice for many back pain sufferers.
When choosing a mattress, consider the firmness scale:
- Soft: Generally not recommended for chronic back pain as it offers insufficient support.
- Medium-Soft: May be suitable for lighter individuals or side sleepers who need more contouring.
- Medium-Firm: Often the ideal choice, providing a balance of support and comfort for most back pain sufferers, especially back and stomach sleepers.
- Firm: Can be beneficial for individuals who need maximum support, but may be too hard for some, leading to pressure points.
“The right mattress should support your body’s natural curves, preventing your spine from sinking or arching unnaturally.”
Pillows
Pillows are essential for supporting the head and neck, which in turn affects the alignment of the entire spine. The best pillow depends on your primary sleeping position.
- Back Sleepers: A medium-thickness pillow that supports the natural curve of your neck is ideal. The pillow should fill the gap between your head and the mattress without pushing your head too far forward. Look for pillows that can be adjusted in height or thickness. A cervical pillow with a contoured shape can also be beneficial.
- Side Sleepers: A firmer, thicker pillow is usually necessary to keep your head and neck aligned with your spine. The pillow should fill the space between your shoulder and your ear. Consider pillows made of denser memory foam or latex that offer good loft and support. A body pillow can also be used between the knees to maintain hip alignment.
- Stomach Sleepers: This position is generally discouraged for back pain sufferers as it can strain the neck and spine. If you must sleep on your stomach, use a very thin, soft pillow or no pillow at all to minimize neck strain. Some find a thin pillow placed under the pelvis helpful to reduce lower back strain.
Pillow materials to consider:
- Memory Foam: Offers excellent support and contouring. Contoured or shredded memory foam pillows can be adjusted for personalized comfort.
- Latex: Provides responsive support and is often more breathable than memory foam.
- Down/Feather: Can be comfortable but may lack sufficient support for consistent spinal alignment.
- Polyester Fill: Inexpensive but tends to flatten over time, losing its supportive qualities.
Finding the Most Comfortable Sleeping Positions
Discovering the optimal sleeping position is a cornerstone of managing chronic back pain, as it directly influences spinal alignment and pressure distribution. While individual needs vary, certain positions have consistently proven more beneficial for alleviating discomfort and promoting restful sleep. This section will guide you through the most effective positions, how to enhance them with supportive aids, and a practical approach to transitioning throughout the night.Understanding how different sleeping positions affect your back is crucial.
The goal is to minimize strain on the spine and surrounding muscles, allowing for natural curvature and reduced inflammation. Experimentation, combined with strategic pillow placement, can unlock significant relief and improve sleep quality.
Beneficial Sleeping Positions for Chronic Back Pain
Certain sleeping postures are widely recommended for individuals experiencing chronic back pain due to their ability to maintain spinal alignment and reduce pressure on sensitive areas. These positions aim to support the natural curves of the spine, preventing unnatural twisting or compression.
- Sleeping on your back (Supine Position): This position is often considered ideal as it allows the spine to rest in a neutral alignment. When performed correctly, it distributes body weight evenly across the widest surface area of your back, minimizing pressure points.
- Sleeping on your side (Fetal Position or Modified Side Sleeping): For many, side sleeping offers a comfortable alternative, especially when properly supported. This position can be particularly helpful for those with herniated discs or spinal stenosis, as it can open up the space between vertebrae.
- Sleeping on your stomach (Prone Position – with caution): While generally discouraged for chronic back pain, some individuals find stomach sleeping to be the only comfortable position. If this is the case, specific modifications are essential to minimize neck and back strain.
Pillow Support for Enhanced Comfort
Pillows are invaluable tools for customizing your sleeping position and providing targeted support to alleviate pressure points. Strategic placement can significantly improve spinal alignment and reduce discomfort, regardless of your preferred sleeping posture.
- For Back Sleepers: Place a small pillow or rolled towel under the natural curve of your lower back to maintain its lordotic curve. A thinner pillow under the head is recommended to keep the neck aligned with the spine. Additionally, a pillow placed under each knee can help reduce pressure on the lower back and hips.
- For Side Sleepers: A firm pillow placed between the knees is crucial to prevent the upper leg from falling forward and twisting the spine. This also helps maintain hip and pelvic alignment. The head pillow should be thick enough to fill the space between the shoulder and the ear, keeping the neck straight. A small pillow can also be placed behind the back for added support and to prevent rolling onto the stomach.
- For Stomach Sleepers (with modifications): If you must sleep on your stomach, place a flat pillow under your pelvis and lower abdomen to lift the hips and reduce the arch in your lower back. Avoid using a thick pillow under your head, as this forces the neck into an unnatural position. A very thin pillow or no pillow at all might be more suitable for the head.
Comparison of Sleeping Positions with Back Pain
Each sleeping position presents unique advantages and disadvantages when dealing with chronic back pain. Understanding these can help you make informed choices about how you rest.
| Position | Pros for Back Pain | Cons for Back Pain |
|---|---|---|
| Back Sleeping | Promotes neutral spinal alignment. Distributes weight evenly. Reduces pressure on the spine. Can be enhanced with knee support. | Can exacerbate snoring and sleep apnea. May not be comfortable for individuals with certain spinal conditions (e.g., severe lordosis). Requires proper head and neck support to avoid strain. |
| Side Sleeping | Can be beneficial for herniated discs and spinal stenosis by opening vertebral space. Allows for natural spinal curve when supported. Good for pregnant individuals. | Can lead to hip and shoulder pain if not properly supported. Risk of spinal misalignment if knees are not kept together. Can cause pressure on the side of the body. |
| Stomach Sleeping | May be the only comfortable position for some individuals. | Significantly strains the neck and upper back due to head rotation. Can flatten the natural curve of the lower back, leading to increased pain. Puts pressure on internal organs. Generally not recommended by medical professionals for back pain. |
Transitioning Between Comfortable Sleep Positions
Moving between sleeping positions during the night is a natural process, especially when experiencing back pain. The key is to do so smoothly and with continued support to minimize any jarring or increased discomfort.
- Prepare your sleep environment: Before settling in, ensure your pillows are strategically placed according to your anticipated positions. Have an extra pillow readily accessible.
- Initiate movement gently: When you feel the need to shift, do so slowly and deliberately. Avoid sudden jerks or twists.
- If rolling from back to side: Bend one knee towards your chest, then gently roll onto your side, placing a pillow between your knees as you settle.
- If rolling from side to back: Slowly unbend your legs and gently roll onto your back, ensuring your head is supported by a pillow. If you were using a knee pillow, readjust it or place it under your lower back if needed.
- If transitioning from stomach to another position: This is often the most challenging. Gently bring your knees towards your chest, then roll to your side, placing a pillow between your knees. From the side, you can then transition to your back if desired.
- Listen to your body: Pay attention to what feels right. If a transition causes discomfort, pause and adjust your position or pillow placement before continuing. The goal is continuous comfort, not a race.
Incorporating Supportive Aids and Techniques

When managing chronic back pain, integrating specific supportive aids and gentle techniques into your bedtime routine can significantly enhance comfort and promote more restful sleep. These tools and practices are designed to alleviate pressure points, maintain proper spinal alignment, and prepare your body and mind for deep relaxation.The strategic use of pillows and gentle preparatory exercises can transform your sleeping experience by offering targeted support and easing muscle tension.
Furthermore, incorporating mindfulness and relaxation techniques can address the mental and emotional aspects of pain, fostering a calmer state conducive to sleep.
Supportive Aids for Enhanced Comfort
Various supportive aids can be utilized to create a more comfortable sleep environment and provide crucial support for a painful back. These items are designed to cushion, align, and reduce pressure on the spine and surrounding muscles.
- Body Pillows: Long, cylindrical, or U-shaped pillows that can be hugged or placed between the legs and behind the back. They offer full-body support, helping to maintain spinal alignment, especially for side sleepers.
- Wedge Pillows: Triangular-shaped pillows that can be used to elevate the upper body or legs. Elevating the upper body can help with acid reflux and reduce pressure on the lower back, while elevating the legs can relieve pressure on the lumbar spine.
- Knee Pillows: Smaller pillows designed to be placed between the knees for side sleepers. This helps to keep the hips, pelvis, and spine in a neutral alignment, preventing the upper leg from pulling the spine out of alignment.
- Lumbar Support Cushions: These can be placed behind the lower back when sleeping on the back or in a reclined position to maintain the natural curve of the spine.
- Adjustable Mattresses: While a larger investment, some mattresses allow for adjustable firmness or elevation, which can be customized to individual needs for back pain relief.
Proper Usage of Pillows for Spinal Support
The effectiveness of pillows in alleviating back pain during sleep depends on their correct placement and application tailored to your sleeping position and specific needs.
Body Pillows
For side sleepers, a body pillow placed between the knees helps to align the hips and pelvis, preventing the upper leg from rotating forward and twisting the lower back. It can also be positioned behind the back to offer additional support and prevent rolling onto the back. For back sleepers, a body pillow can be placed along the side of the body to prevent accidental rolling onto the stomach, which can strain the back.
Wedge Pillows
When using a wedge pillow to elevate the upper body, it should be positioned under the torso, allowing the head and neck to rest comfortably on a separate pillow. This angle can reduce pressure on the lumbar spine and alleviate symptoms of GERD. For leg elevation, a smaller wedge or stacked regular pillows can be placed under the knees while lying on the back.
This position helps to decrease the strain on the lower back by reducing the arch in the lumbar spine.
Knee Pillows
A knee pillow is primarily for side sleepers. It should be placed snugly between the knees, ensuring it is thick enough to keep the knees slightly separated and the hips aligned. For those who sleep on their back, a knee pillow can be placed under the knees to help maintain the natural curve of the lower back and reduce strain.
Gentle Pre-Bedtime Stretching and Movement
Incorporating gentle stretching or light movement before sleep can significantly ease back pain by releasing muscle tension and improving flexibility. These activities should be performed slowly and with care, avoiding any movements that cause sharp pain.
Pre-Sleep Stretches
A routine of gentle stretches can prepare the body for rest and reduce discomfort.
- Knee-to-Chest Stretch: Lie on your back and gently bring one knee towards your chest, holding for 20-30 seconds. Repeat with the other leg, then try both knees simultaneously if comfortable. This helps to stretch the lower back muscles.
- Pelvic Tilts: Lie on your back with knees bent and feet flat on the floor. Gently flatten your lower back against the mattress by tightening your abdominal muscles and tilting your pelvis upward. Hold for a few seconds and release. This strengthens abdominal muscles and gently massages the lower back.
- Cat-Cow Stretch (Modified): On your hands and knees, gently arch your back upwards like a cat, tucking your chin to your chest. Then, gently let your back sag downwards, lifting your head slightly (like a cow). Move slowly and fluidly between these two positions. This improves spinal mobility.
- Child’s Pose: Kneel on the floor, sit back on your heels, and fold your torso forward, resting your forehead on the floor. Extend your arms forward or rest them alongside your body. This pose gently stretches the back and hips.
Light Movement
A short, slow walk before bed can also be beneficial. Even a 10-15 minute stroll at a relaxed pace can help to loosen muscles and improve circulation without exacerbating pain. Avoid strenuous activity close to bedtime.
Mindfulness and Relaxation Exercises for Restful Sleep
Preparing the body and mind for sleep is crucial when dealing with chronic back pain. Mindfulness and relaxation techniques can help to calm the nervous system, reduce anxiety associated with pain, and promote a state of deep relaxation conducive to sleep.
Mindfulness Techniques
Mindfulness involves focusing your attention on the present moment without judgment. This can help to detach from the discomfort of pain and reduce the mental distress it causes.
- Body Scan Meditation: Lie down comfortably and systematically bring your attention to different parts of your body, noticing any sensations without trying to change them. This practice can increase awareness of physical tension and promote relaxation.
- Mindful Breathing: Focus on the sensation of your breath as it enters and leaves your body. Notice the rise and fall of your chest or abdomen. When your mind wanders, gently guide your attention back to your breath. This simple technique can anchor you in the present and calm the mind.
Relaxation Exercises
These techniques aim to actively reduce physical and mental tension.
- Progressive Muscle Relaxation (PMR): This involves tensing and then releasing different muscle groups in your body. Start with your toes and systematically work your way up, noticing the difference between tension and relaxation. This can help to release deep-seated muscle tension that contributes to back pain.
- Guided Imagery: Imagine yourself in a peaceful and calming place, engaging all your senses. Focus on the sights, sounds, smells, and feelings associated with this tranquil environment. This can help to distract from pain and induce a state of deep relaxation.
- Listening to Calming Audio: Soft music, nature sounds, or guided relaxation scripts played at a low volume can create a soothing atmosphere that aids in falling asleep.
Lifestyle Adjustments for Better Sleep and Reduced Pain
Making conscious adjustments to your daily lifestyle can significantly impact your ability to sleep comfortably with chronic back pain. These adjustments address how your everyday activities, posture, and diet contribute to or alleviate discomfort during the night. By integrating these changes, you can create a more supportive environment for your back, both during waking hours and while you rest.The connection between our daily habits and nighttime comfort is profound.
Understanding this relationship allows us to proactively manage our back pain. Small, consistent changes can lead to substantial improvements in sleep quality and overall well-being.
Impact of Daily Activities and Posture on Nighttime Back Pain
The way we move and hold ourselves throughout the day directly influences the strain placed on our spine. Prolonged sitting, improper lifting techniques, and habitual slouching can all lead to muscle fatigue, stiffness, and increased inflammation, which often manifest as heightened back pain when lying down. Even seemingly minor activities, when performed with poor posture, can accumulate stress on the back over time.To mitigate this, it is crucial to be mindful of your posture in all activities.
This includes how you sit at your desk, stand while waiting, and even how you walk. Regular movement breaks are essential to prevent muscles from becoming overly fatigued and stiff.
Ergonomic Adjustments in Daily Routines
Implementing ergonomic principles into your daily life can create a significant difference in managing back pain. This involves modifying your environment and your approach to tasks to reduce physical stress.Here are some key ergonomic adjustments to consider:
- Workstation Setup: Ensure your desk chair provides adequate lumbar support, and your computer screen is at eye level to prevent neck and back strain. When standing, maintain a slight bend in your knees and avoid locking them.
- Lifting Techniques: Always bend your knees and keep your back straight when lifting objects. Engage your core muscles and lift with your legs, not your back.
- Movement and Breaks: If your job involves prolonged sitting or standing, schedule regular breaks to walk around, stretch, and change your position. Even a few minutes of gentle movement can help relieve pressure on your spine.
- Driving Comfort: Adjust your car seat to support your lower back, and consider using a lumbar support cushion if needed. Take breaks during long drives to get out and stretch.
Dietary Considerations for Reduced Inflammation and Improved Sleep
The foods we consume play a vital role in managing inflammation throughout the body, which is often a significant contributor to chronic back pain. An anti-inflammatory diet can help reduce pain levels, thereby promoting more restful sleep.A balanced diet rich in certain nutrients can be particularly beneficial:
- Omega-3 Fatty Acids: Found in fatty fish (salmon, mackerel), flaxseeds, and walnuts, these have potent anti-inflammatory properties.
- Antioxidants: Fruits and vegetables, especially berries, leafy greens, and colorful vegetables, are packed with antioxidants that combat cellular damage and inflammation.
- Whole Grains: Opt for whole grains like oats, quinoa, and brown rice over refined grains, as they provide sustained energy and fiber.
- Hydration: Staying well-hydrated is crucial for maintaining healthy bodily functions, including joint lubrication and tissue health.
Conversely, limiting processed foods, excessive sugar, and unhealthy fats can help reduce overall inflammation.
Importance of Consistent Sleep Schedules
Establishing and maintaining a consistent sleep schedule is a cornerstone of effective pain management and improving sleep quality with chronic back pain. Going to bed and waking up around the same time each day, even on weekends, helps regulate your body’s natural sleep-wake cycle, known as the circadian rhythm.Disruptions to this rhythm can exacerbate pain sensitivity and make it harder to fall asleep and stay asleep.
A predictable sleep schedule signals to your brain and body when it’s time to wind down and rest, promoting deeper, more restorative sleep.
A consistent sleep schedule reinforces your body’s natural sleep-wake cycle, leading to more predictable pain management and improved sleep quality.
This regularity can help reduce the intensity and frequency of pain flares, making it easier to find comfortable sleeping positions and achieve the rest your body needs to heal and recover.
When to Seek Professional Guidance

While many strategies can be employed at home to improve sleep comfort with chronic back pain, recognizing when professional help is necessary is crucial for effective management and long-term well-being. Persistent or worsening symptoms, or pain that significantly impacts daily life, are strong indicators that medical consultation is warranted.Understanding the nuances of chronic back pain and its effect on sleep can be complex, and a healthcare professional can provide personalized assessments and treatment plans.
They can help differentiate between common discomfort and more serious underlying conditions, ensuring you receive the most appropriate care.
Signs and Symptoms Indicating a Need for Medical Consultation
It is important to be aware of certain red flags that suggest your back pain and its impact on sleep require professional medical attention. These symptoms may indicate an underlying issue that needs diagnosis and treatment beyond self-management strategies.
- Sudden or severe back pain that prevents you from standing up straight or moving.
- Back pain accompanied by fever, unexplained weight loss, or chills.
- Numbness, tingling, or weakness in your legs, feet, or groin area.
- Loss of bowel or bladder control.
- Pain that radiates down one or both legs, especially below the knee.
- Back pain that is worse at night or wakes you from sleep and does not improve with rest.
- Pain that persists for more than a few weeks despite home care measures.
- Pain that significantly interferes with your daily activities, work, or social life.
Types of Healthcare Professionals for Back Pain Management
A multidisciplinary approach is often beneficial for managing chronic back pain that disrupts sleep. Various healthcare professionals can offer specialized expertise and support.The following professionals can play a vital role in diagnosing, treating, and managing chronic back pain affecting sleep:
- Primary Care Physician (PCP): Your first point of contact, who can perform an initial assessment, rule out common causes, and refer you to specialists.
- Orthopedic Surgeon: Specializes in the musculoskeletal system and can diagnose and treat bone, joint, and muscle conditions.
- Neurosurgeon: Focuses on conditions affecting the nervous system, including the spinal cord and nerves, which can be involved in back pain.
- Physiatrist (Physical Medicine and Rehabilitation Physician): Specializes in diagnosing and treating conditions affecting nerves, muscles, and bones, often focusing on non-surgical treatments and rehabilitation.
- Rheumatologist: Deals with inflammatory conditions of the joints, muscles, and bones, such as arthritis, which can cause back pain.
- Pain Management Specialist: Physicians trained to diagnose and treat chronic pain conditions using a variety of methods, including medication, injections, and interventional procedures.
- Physical Therapist: Develops customized exercise programs to improve strength, flexibility, posture, and reduce pain.
- Chiropractor: Provides manual adjustments and other therapies to the spine and joints.
- Sleep Specialist: If sleep disruption is the primary concern and back pain is secondary, a sleep specialist can help diagnose and manage sleep disorders.
Common Diagnostic Approaches for Back Pain Affecting Sleep
Healthcare providers utilize a range of diagnostic tools and techniques to accurately identify the cause of back pain that is impacting sleep. A thorough evaluation is essential for developing an effective treatment plan.The diagnostic process typically involves several key components:
- Medical History: A detailed discussion about your pain, its onset, duration, intensity, aggravating and alleviating factors, and any associated symptoms. Your sleep patterns and how the pain affects them will be a significant part of this discussion.
- Physical Examination: This involves assessing your posture, range of motion, muscle strength, reflexes, and palpating the spine and surrounding muscles to identify areas of tenderness or dysfunction.
- Imaging Tests:
- X-rays: Useful for visualizing bones and identifying fractures, arthritis, or significant spinal alignment issues.
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues, including discs, nerves, and the spinal cord, helping to detect herniated discs, spinal stenosis, or tumors.
- CT Scan (Computed Tomography): Offers cross-sectional images of the spine, often used when MRI is not suitable or to get more detail on bony structures.
- Nerve Conduction Studies (NCS) and Electromyography (EMG): These tests assess the function of nerves and muscles to detect nerve damage or pinched nerves.
- Blood Tests: May be ordered to rule out inflammatory conditions, infections, or other systemic diseases that could be contributing to back pain.
Potential Treatment Options Recommended by Healthcare Providers
Once a diagnosis is established, a healthcare provider will recommend a personalized treatment plan to address your chronic back pain and improve your sleep. These options often involve a combination of approaches.Treatment strategies can include:
- Medications:
- Over-the-counter pain relievers: Such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen.
- Prescription pain relievers: Stronger NSAIDs, muscle relaxants, or neuropathic pain medications if nerve involvement is suspected.
- Topical pain relievers: Creams, gels, or patches applied to the skin.
- Physical Therapy: A cornerstone of back pain management, involving exercises for strengthening core muscles, improving flexibility, posture correction, and manual therapy techniques.
- Injections:
- Epidural steroid injections: To reduce inflammation around nerve roots.
- Facet joint injections: To numb pain in the small joints of the spine.
- Trigger point injections: To relieve localized muscle pain.
- Lifestyle Modifications: Recommendations for weight management, smoking cessation, ergonomic adjustments at work and home, and stress reduction techniques.
- Assistive Devices: Such as specialized pillows, mattress toppers, or bracing, as discussed previously, to support comfortable sleeping positions.
- Mind-Body Therapies: Techniques like mindfulness, meditation, cognitive behavioral therapy (CBT) for pain, and yoga can help manage pain perception and improve coping mechanisms.
- Surgery: Considered a last resort for severe cases unresponsive to conservative treatments, addressing structural issues like significant disc herniation or spinal stenosis.
Conclusive Thoughts
In conclusion, navigating the challenges of sleeping comfortably with chronic back pain is an achievable goal with the right knowledge and approach. By understanding the root causes of your discomfort, optimizing your sleep environment, adopting beneficial sleeping positions, utilizing supportive aids, and making mindful lifestyle adjustments, you can significantly improve your sleep quality and overall well-being. Remember, consistent effort and seeking professional guidance when needed are key to transforming your nights from a source of pain to a sanctuary of rest and rejuvenation.